Perceived health benefits (there are none)
Module 2
What is FGM?
By the end of the module, you will have an understanding of FGM, the implications, reasons for the practice, and assessing the risk to girls and women.

2.1 Background to FGM

Definition and criteria for harm
FGM is a crime in the UK. FGM is defined in the FGM Act 2003 as 'excision, infibulation or otherwise mutilation the whole, or part of a girls labia majora, labia minora or clitoris'
"I bled. Bled so much. When it happened to me... after... when I had my children. I bled every time. With every bleed, it was a reminder that I had FGM done to me. I didn't choose for it to happen. It happened to me."
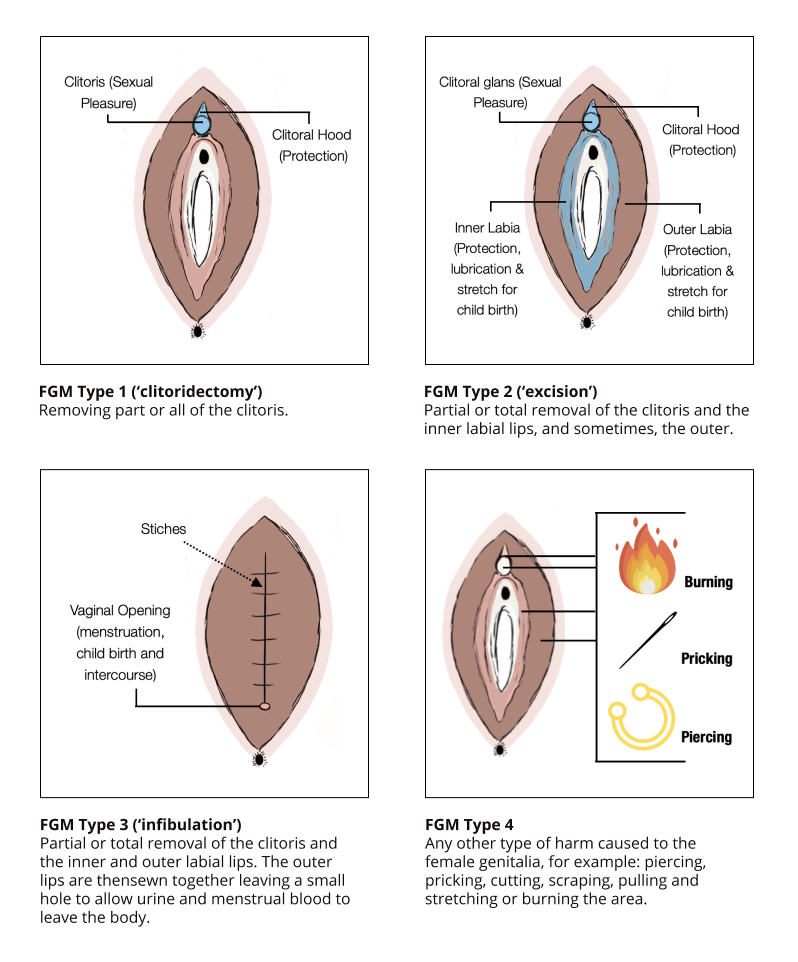
According to the World Health Organisation, the four types of FGM are defined as:
Type 1: Clitoridectomy: Partial or total removal of the clitoral glans (the external and visible part of the clitoris) and/or the prepuce/clitoral hood (the fold of skin surrounding the clitoral glans).
Type 2: Excision: Partial or total removal of the clitoral glans and the labia minora (the inner folds of the vulva), with or without removal of the labia majora (the outer folds of skin of the vulva).
Type 3: Infibulation: Narrowing of the vaginal opening with the creation of a covering seal. This is done by cutting and repositioning the labia minora, or labia majora.
Type 4: Other harm to the genitalia: All other harmful procedures to the female genitalia for non-medical purposes, for example pricking, piercing, incising, scraping, cauterising, labial elongation
FGM violates children’s rights as defined in the United Nations Convention on the Rights of the Child (UNCRC):
- The right to be free from discrimination (Article 2);
- The right to be protected from all forms of mental and physical violence and maltreatment (Article 19(1));
- The right to highest attainable standard of health (Article 24);
- The right of freedom from torture or other cruel, inhuman or degrading treatment or punishment (Article 37).
A girl’s or woman’s FGM will look different. To establish what type of FGM a girl or woman has had, a medical examination will be needed.
FGM cannot be 'reversed'. Once the procedure has been carried out, and parts of the external genitalia have been removed, their functions are either depleted or diminished.
However, in type 3 FGM, girls or women can undergo a procedure called 'de-infibulation. Deinfibulation refers to cutting open the sealed vaginal opening to allow sexual intercourse or to facilitate childbirth.

Terminology
FGM is sometimes referred to as FGC, or female genital cutting, however has many other names or teminology recognised across various languages and communities. FGM is not mandated by any religion.
Some of the other names can be found in this free download: https://nationalfgmcentre.org.uk/wp-content/uploads/2018/02/FGM-Terminology-for-Website.pdf
It is important for practitioners to consider the use of their language when addressing FGM with families. Some words for FGM denote that the practice is positive. It is therefore important for practitioners to explore the meaning of words with families, and introduce words like 'mutilation' to explain the severity of the practice. Moreover, the term female circumcision should be avoided as it draws a parallel with male circumcision and, as such conflates the two very distinct practices.
Why does FGM happen?
FGM is a deeply entrenched social norm rooted in gender inequality. Many affected communities believe that FGM is a necessary custom to ensure that a girl is accepted within the community and eligible for marriage. Families who practice FGM on girls usually see it as a way of safeguarding their future.
It is important to remember that no matter the justification, FGM is a gross violation of the rights of girls and women:
- FGM violates the Rights of the Child (UNCRC)
- FGM violates the principles of non-discrimination (UNCEDAW)
- FGM violates a girl or womans right to life (when the procedure results in death) and adequate health (UNDHR)
- FGM violates a girl or womans right to freedom from torture or cruel, inhuman or degrading treatment or punishment (UNCAT)
2.2 Global prevalance

Worldwide statistics
According to UNICEF, the exact number of girls and women worldwide who have undergone FGM is unknown, due to a lack of available data and the overall clandestine nature of the practice, however it is known that at least 200 million girls and women aged 15–49 from 31 countries have been subjected to the practice, and a further 3 million girls are at risk globally every year.
Data available from research show that FGM is prevalent in countries from the Atlantic coast to the Horn of Africa, in areas of the Middle East, Asia, Latin America and Russia - the only continent not affected by FGM is Antarctica.
'Practicing' vs 'affected' communities. Not all communities within countries are affected by FGM. It is therefore important not to label all communities as 'practicing. Moreover, recognising communities as 'affected' acknowledges that there is power in ending the practice.
As mentioned in module 1, there are also variations in the type of FGM across communities, the number of affected communities within countries and regions, and circumstances around how FGM is performed.
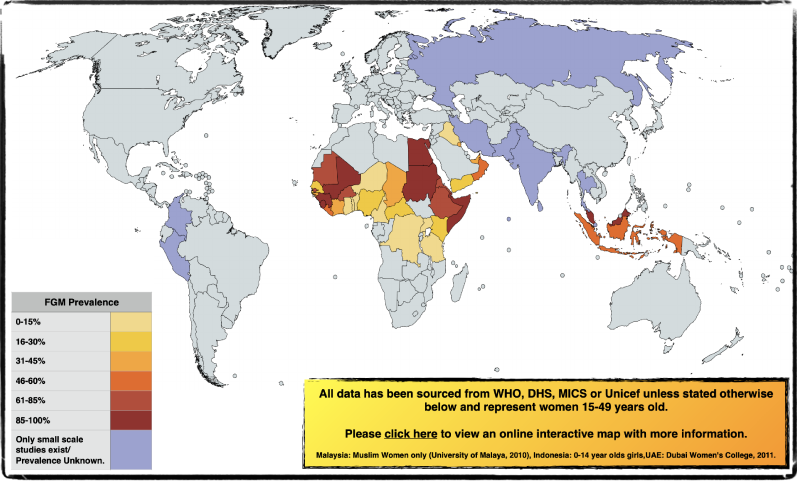
Click here to access our interactive FGM prevalence map.
According to UNICEF, here has been an overall decline in the prevalence of FGM over the last three decades, going from 1 in 2 girls having undergone FGM (15-49) to 1 in 3 (15-49), but not all countries have made progress in the same ways and the pace of decline has been uneven
Prevalence in England and Wales
Statistical Estimates:
An estimated 103,000 women aged 15-49 with FGM born in countries in which it is practised were living in England and Wales in 2011, compared with the estimated 66,000 in 2001.
In addition there were an estimated 24,000 women aged 50 and over with FGM born in FGM practising countries and nearly 10,000 girls aged 0-14 born in FGM practising countries who have undergone or are likely to undergo FGM.
Over half of the women aged 15-49 with FGM, 53,000, were born in countries with almost universal Type III FGM, and a further 20,500 were born in countries with very high rates of Type I and II FGM.
Prevalence rates varied considerably by region, with London having by far the highest prevalence at 21.0 per 1,000 population.
The highest rates were in London boroughs, with 47.4 per 1,000 in Southwark and 38.9 per 1,000 in Brent.
Outside London, Manchester, Slough, Bristol, Leicester and Birmingham had high prevalence rates, ranging from 12 to 16 per 1,000.
Other authorities, including Milton Keynes, Cardiff, Coventry, Sheffield, Reading, Thurrock, Northampton and Oxford had rates of over 7 per 1,000.
Many mainly rural areas had prevalences well below one per 1,000, but above zero.
There are no local authorities areas in England and Wales unaffected by FGM.
The Serious Crime Act 2015 made the recording of newly identified cases of FGM by healthcare providers in England mandatory. The recording in the settings highlighted relates to a NHS England direction. Section 74 SCA 2015 relates to mandatory reporting by regulated professionals - Health, Social Care and Education professionals in young people under 18 years relating to known cases of FGM, including acute hospital providers, mental health providers and GP practices, mandatory. Since the collection began, NHS trusts and GP practices have reported information about 30,335 individual women and girls. Between April 2015 and March 2022 there were a total of 74,875 attendances for these individuals where FGM was identified.
Child In Need Census Data
The Department for Education encourages local authorities within the Child in Need Census Data to record factors identified at the end of assessment - which are factors that social workers record as being relevant in a case. Although not all episodes have factors recorded, the data from 2016-2021 shows that there were 4,900 cases where FGM was recorded as a factor within an assessment.
2.3 Health consequences

Physical impacts
Some of the health consequences of FGM include:
- Death
- Death of the mother and/or baby during childbirth
- Severe pain and shock
- Hemorrhaging
- Injury to adjacent tissue
- Urine retention
- Increased risk of HIV and AIDS
- Uterus, vaginal and pelvic infections
- Cysts and neuromas
- Increased risk of fistula, including obstetric fistula (A hole between the birth canal and bladder and/or rectum)
- Complications in childbirth, such as tearing
- Sexual dysfunction
- Difficulties in menstruation
- Infertility
"I remember that day. Being led up the stairs. So many people around... who I don't remember. And then it happened. I don't like to get into lifts now, or be around too many people. It brings me back to that day."
It is important to remember that all types of FGM can cause life long health consequences to girl's and women's health. The removal of a 'greater' amount of labial tissue does not dictate the severity of the harm FGM causes, and the impact it can have on a girl or woman's life. It is also important to remember that not all women will report experiencing physical or mental health consequences as a result of undergoing FGM, and that every girl or woman should be treated as an individual.
According to UNICEF, around 1 in 3 adolescent girls (15-19 years) who have undergone FGM were cut by health professional.
The medicalisation of FGM
In many countries, there has been a rise in the medicalisation of FGM, where trained health-care professionals, in public or private clinics, at home or elsewhere are perfoming FGM on girls. Some have wrongly deemed this to be 'safer' than performing FGM in more 'traditional' settings - leading to reduced complications. It is important to remember that health-care professionals who perform FGM are violating girls’and women’s rights to life, physical integrity and health, and are instead promoting a cloak of legitimacy of the practice. They also violate medical ethnics of providing the highest quality of health care possible. Medicalising FGM does not make it safer, as the practitioner is still removing healthy tissue, for no medical reason, interfering with the natural functions of girls’ and women’s bodies.
According to the World Health Organisation, treatment of the health complications of FGM in 27 'high prevalence countries' is estimated to cost 1.4 billion USD per year and is projected to rise to 2.3 billion USD by 2047 if no action is taken
Prevalence
According to UNICEF, around 1 in 3 adolescent girls (15-19 years) who have undergone FGM were cut by health professional.
According to the World Health Organisation, treatment of the health complications of FGM in 27 'high prevalence countries' is estimated to cost 1.4 billion USD per year and is projected to rise to 2.3 billion USD by 2047 if no action is taken.

Why has there been a trend towards the rise in medicalised FGM?
- Belief that it could be a 'safer' alternative method
- Financial incentive for the health professonal
- Belief that it is a step towards abandoning FGM
Why has there been a trend towards the rise in medicalised FGM?
- Some wrongly believe it could be a 'safer' alternative method
- There can be a financial incentive for the health professonal
- Some believing that it is a step towards abandoning the practice altogether
Emotional impacts
Some studies have also found that FGM can be associated with mental health connected with exposure to traumatic events. These can include:
- Irritability and frustration
- Flashbacks
- PTSD
- Self-harm, suicidal thoughts or intent
- Nightmares
- Low self-esteem
- Depression and post-natal depression
- Intense feelings of fear and helplessness
- Perceptions of the body which are negative (body dysmorphia)
- Paranoia
- Anxiety
- Flashbacks in response to touch
- Claustraphobia (where women report a large number of people present when they underwent FGM)
- Psychosexual problems
Exploring your service user/client/patient's emotional wellbeing:
It is important to explore every girl or woman's emotional wellbeing to establish the most appropriate support they can access. Reassure your service user/client/patient who is experiencing complications as a result of FGM that this is common, and moreover that mental health conditions can be present too.
To read more about the health consequences of FGM, please see our 'health infographic' - https://nationalfgmcentre.org.uk/wp-content/uploads/2022/03/FGM-and-Health-Consequences-Infographic-2022.pdf
2.4. Risk Indicators

Significant risk factors
- Mother has requested re-infibulation following childbirth
- A girl has an older sibling or cousin who has undergone FGM
- One or both parents consider FGM integral to their cultural or religious identity
- Physical signs that FGM has been carried out
- Parent/carer/another trusted adult has enquired or stated that they want FGM performed
- Parent/carer indicate that they have limited understanding of the harm of FGM
- Parent/carer indicate that they have limited understanding of the law in relation to FGM
- The family indicate that there are strong levels of influence held by pro-FGM elders who are involved in bringing up female children and they feel powerless to say no
- A girl confides that she is to have a ‘special procedure’ or to attend a special occasion to ‘become a woman’
Access the Risk Assessment sheet here: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/576051/FGM_risk_assessment_templates.pdf
Potential risk factors
The list below is not exhaustive, and there could be additional risk factors, potentially related specifically to a particular community. For example, if FGM is associated to when a girl reaches a particular age.
Harmful practices often co-exist
The ways in which different harmful practices intersect and diverge varies. For example, in some communities where FGM is prevalent, early forced marriage is common too. Both are grounded in gender norms that devalue girls and have been used to control female sexuality. FGM is also sometimes linked to beliefs in witchcraft or evil spirits. This can manifest as a belief that the harmful health consequences of FGM are attributable to witchcraft, and/or that the person performing FGM has supernatural powers.
Therefore, in cases where there are concerns for FGM, it’s important to be professionally curious about the occurrence of other harmful practices.
It is important that professionals build a picture of risk within an assessment, giving consideration to risk as well as potential strengths in cases. A helpful way to do this is to consider:
- What are you or the family worried about, in terms of actual harm, and risk of significant harm or danger of FGM to the girl(s)?
- What are the family’s strengths and what protective/safety factors do they have in place to protect their daughter(s) from FGM?
- What needs to happen to effect change? What does the family need to demonstrate/do, now and in the future to show that they can keep the girl(s) safe from FGM? What do you as a professional need to do to support the family in achieving their safety goals/plan?
Welcome to your short assessment for module 2! Complete this case study to test your knowledge.